Τι πρέπει να γνωρίζω
Μάθετε για τις χρήσεις των βλαστοκυττάρων
Ενημερωτικό Υλικό
Μάθετε για τις χρήσεις των βλαστοκυττάρων
Κλείστε ραντεβού εδώ
Ενημερωθείτε υπεύθυνα για τα βλαστοκύτταρα
Development of autologous immunotherapies for cancer and leukemia from umbilical cord blood
Biohellenika R&D developed cancer immunotherapy protocols with autologous hematopoietic cord blood stem cells. Immunotherapies are personalized and targeted treatments, which are used in combination with other drugs to effectively treat cancer. Today 44 clinical trials are using umbilical cord blood to create immunotherapies for cancer, lymphomas and leukemia, while recently it has been announced that immunotherapies have reduced classic allogeneic hematopoietic transplants by 50%. Immunotherapies using autologous umbilical cord blood are based on the creation of dendritic cells, which are specialized for the specific malignancy antigens of the individual patient. Umbilical cord blood has an advantage over other sources, because it provides the largest number of highly active dendritic cells in a short time. Biohellenika's R&D developed a colon cancer immunotherapy protocol from umbilical cord blood. This treatment was tested on a colon cancer cell line and was highly effective. This protocol was published in the international journal, Differentiation 125 (2022) 54-61, and the company subsequently funded the development of a new immunotherapy protocol to treat leukemias. This protocol concerns the treatment of Acute Myeloid Leukemia, which usually appears after 60 years of life and the survival of patients with the usual treatments is short.
Japan approves new stem cell-based Alzheimer's therapy
19:28 18 Jan 2024
In what could be a major breakthrough for Alzheimer's treatment, the Japanese Ministry of Health and Welfare has given the greenlight to a regenerative medicine technology based on administering fat-derived stem cells intravenously and into the spinal cord.
Developed by Korea's leading adult stem cell research institute, Biostar Stem Cell Research Institute, this new stem cell therapy involves administering 150-250 million stem cells intravenously and a further 50 million into the spinal cord cavity five times at intervals of two to four weeks.
“This is the first step in our project to overcome Alzheimer’s, which was launched with our commitment to conquer this disease,” Biostar Stem Cell Research Institute director Dr. Jeong-Chan Ra said.
“With the start of stem cell treatment, Biostar will support Alzheimer’s patients from all over the world – including Japan, Korea, China, and the US, starting in Japan – to restore their memory and ultimately their humanity.”
There are over 10 million new cases of dementia each year globally, with Alzheimer’s being the most common cause of the neurodegenerative disease.
Unlike most treatments for Alzheimer’s, which are limited to slowing the progression of disease, stem cell therapies are expected to offer a functional cure.
Testing on mice models revealed stem cell therapies offer a multi-pronged path of attack against Alzheimer's.
Mice who received the stem cell treatment improved in vital ways – cerebral vascular regeneration, and brain cell protection and regeneration were all observed following treatment, which also mediated the IL-10 cytokine.
IL-10 plays a central role in inflammation and neurological protection responses, particularly relevant given inflammation is considered to be one of the core contributors to cognitive decline.
An article by the BioSpectrum Bureau, a media platform for the healthcare and bioscience industry in the Asia Pacific region, stated: “No other compound or treatment has ever suggested so strongly the potential to prevent, as well as stop, this epidemic of incurable dementia sweeping across suffering patients and their families.”
Treatment has already begun at the Shinjuku Clinic in Tokyo, providing a sorely needed treatment pathway for those suffering from Alzheimer's.
«Υλοποιήθηκε στο πλαίσιο της Δράσης ΕΡΕΥΝΩ – ΔΗΜΙΟΥΡΓΩ - ΚΑΙΝΟΤΟΜΩ και συγχρηματοδοτήθηκε από το Ευρωπαϊκό Ταμείο Περιφερειακής Ανάπτυξης (ΕΤΠΑ) της Ευρωπαϊκής Ένωσης και εθνικούς πόρους μέσω του Ε.Π. Ανταγωνιστικότητα, Επιχειρηματικότητα & Καινοτομία (ΕΠΑνΕΚ) (κωδικός έργου: T1ΕΔΚ-04567)»
Στα πλαίσια του έργου ArthroMicroPerMed- T1ΕΔΚ-04567 συνδυάζονται η εξατομικευμένη ιατρική θεραπεία (PersonalizedMedicin) για φθορές αρθρώσεων (Arthro) με ταυτόχρονη έγχυση νέων "ευφυών" βιοϋλικών και βλαστοκυττάρων απομονωμένων από ισχίο ή γόνατο για "αρθρο-νέο-γένεση" καθώς επίσης η μελέτη επίδρασης μεταβολιτών τουμικροβιώματος (Micro) στην γένεση της οστεοαρθρίτιδας.
Παρασκευάστηκαν βιο-ικριώματα με πρωτεϊνική μηχανική τα οποία συνδυάζουν την ελαστικότητα και την μηχανική αντοχή ελαστίνης και φιβροϊνης του μεταξιού, αντίστοιχα.
Τα"ευφυή" βιοϋλικά είναι επαναλαμβανόμενα μοτίβα πορώδεις διασυνδεδεμένες υδροπηκτές αποτελούμενες από συγκεκριμένων περιοχών των προαναφερθέντων πρωτεϊνών ("recombinamer"), με ικανότητα "αυτο-οργάνωσης" και σε σύντηξη με
α) πεπτίδια της ΒΜP7 (BoneMorphogenetic Protein-7) και του TGFb (Transforming Growth Factor b) που προάγουν τη χονδρογένεση, και με
β) πεπτίδια κολλαγόνου και λαμινίνης – γνωστά από τη διεθνή βιβλιογραφία- για την προσέλκυση των ομόλογων βλαστοκυττάρων. Το υλικό αυτό είναι ενέσιμο και διαθέτει επιπρόσθετα "θέσεις" αλληλεπίδρασης ηπαρίνης, απαραίτητου συστατικού της εξωκυττάριας μήτρας (ECM).
Η καινοτομία αυτών των "ευφυών" υλικών έγκειται επίσης στην ιδιότητά τους να "προειδοποιούν" για βακτηριακές μολύνσεις με αλλαγή χρώματος της υδροπηκτής μέσω του βιομιμητικού πολυμερικού αισθητήρα ο οποίος αποτελείται από λιπιδικά νανοσωματίδια που εσωκλείουν poly-diacetylene (PDA) και φθορίζουσες χρωστικές, συστατικά μη τοξικά για τα κύτταρα και τον οργανισμό γενικότερα.
Τα καινοτόμα αυτά ικριώματα επάγουν την χονδρογένεση μεσεγχυματικών κυττάρων τόσο σε κυτταροκαλλιέργειες όσο και μετά την έγχυσή τους με μεσεσεγχυματικά κύτταρα -παρασκευασμένα από την συμμετέχουσα εταιρεία BioHellenika -σε γόνατο/ισχίο μικρών ζώων.
Μία άλλη σημαντική καινοτομία του ArthroMicroPerMed είναι η μελέτη της επίδρασης του μικροβιώματος τόσο στα νέα βιομιμητικά υλικά όσο και στην πρόληψη /"εξατομικευμένη θεραπεία" της οστεοαρθρίτιδας (ΟΑ). Η μελέτη της επίδρασης συγκεκριμένων βακτηριακών μεταβολιτών SCFA (Short Chain Fatty Acids) μικρής αλυσίδας λιπαρών οξέων σε πιθανή γένεση / εξέλιξη της νόσου έγινε με μικρο-βιο-αντιδραστήρα που κατασκευάστηκε από την συμμετέχουσα εταιρεία BD Inventions και επιτρέπει την ταυτόχρονη ανάπτυξη βακτηρίων σε συνθήκες βέλτιστης ανάπτυξής τους και χονδροκυττάρων σε παρακείμενες διαχωριζόμενες μικροκυψελίδες.
Η καταλληλότητα και η αποτελεσματικότητα των βιο-ικριωμάτων μελετήθηκε και με in vivo προγραμματισμένες κλινικές μελέτες σε μικρά ζώα με οστεοαθρίτιδα με έγχυση του καινοτόμου υλικού και παρακολούθηση/μελέτη πορείας της θεραπείας.

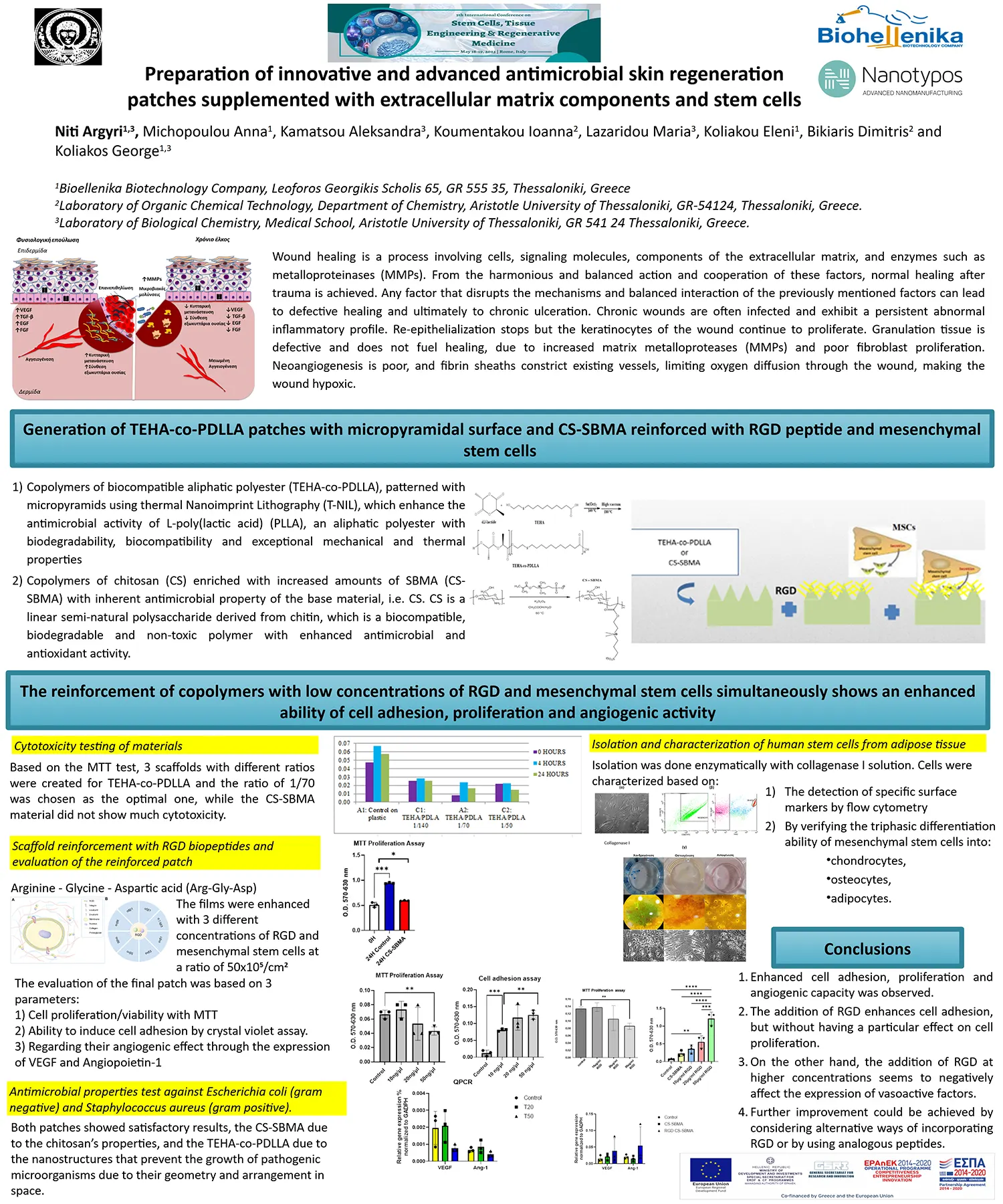
Preparation of innovative and advanced antimicrobial skin regeneration patches supplemented with extracellular matrix components and stem cells T6YVP-00288 with the co-funding of Greece and European Union
Preparation of innovative and advanced skin regeneration patches with inherent antimicrobial activity supplemented with extracellular matrix components and stem cells.
Today, regeneration and healing of the skin occurs mainly through invasive methods, which are painful, time consuming, costly and stressful for patients. A new trend in the healing of skin wounds is the use of hydrogel-type polymeric patches which maintain a moisture level suitable for tissue regeneration.
However, these patches trap moisture in the skin, which, while it is necessary for tissue growth, is also an agent for the growth of microbes. To address this, antimicrobial drugs have been used but they were found to slow down the regeneration of skin tissue. Thus, the development of innovative polymeric patches whose molecules carry antimicrobial compounds or possess antimicrobial topography are a promising solution to this problem.
BIOHELLENIKA biotechnology company, with years of experience in the stem cell field and research on cellular therapies and modern equipment on its premises, NANOTYPOS O.E. nanoprint lithography research and development company, with extensive know-how in nano- production processes and innovative facilities, and the team of Professor Bikiaris with the necessary experience and the appropriate laboratory equipment for the development of new advanced polymeric materials, are working together to:
Project Coordination: BIOHELLENIKA (Dr. George Koliakos, MD)
Principal Investigator: Dr Kokkona Kouzi-Koliakou, MD
Duration: 1/05/2020-27/08/2023
4/12/2023
Stem cell-based treatment controls blood sugar in people with Type 1 diabetes
November 27, 2023
University of British Columbia
:
An innovative stem cell-based treatment for Type 1 diabetes can meaningfully regulate blood glucose levels and reduce dependence on daily insulin injections, according to new clinical trial results. The therapy aims to replace the insulin-producing beta cells that people with Type 1 diabetes lack. Dubbed VC-02, the small medical implant contains millions of lab-grown pancreatic islet cells, including beta cells, that originate from a line of pluripotent stem cells.
An innovative stem cell-based treatment for Type 1 diabetes can meaningfully regulate blood glucose levels and reduce dependence on daily insulin injections, according to new clinical trial results from the University of British Columbia (UBC) and Vancouver Coastal Health (VCH).
"This is a significant step toward a functional cure for Type 1 diabetes," said Dr. David Thompson, principal investigator at the Vancouver trial site, clinical professor of endocrinology at UBC and director of the Vancouver General Hospital Diabetes Centre. "For the first time, a stem cell-based device can reduce the amount of insulin required for some trial participants with Type 1 diabetes. With further refinement of this approach, it's only a matter of time until we have a therapy that can eliminate the need for daily insulin injections entirely."
The findings, published today in Nature Biotechnology, arise from a multicenter clinical trial for an experimental cell therapy developed by U.S. biotechnology company ViaCyte (acquired by Vertex Pharmaceuticals) that is being clinically tested in Canada.
The therapy aims to replace the insulin-producing beta cells that people with Type 1 diabetes lack. Dubbed VC-02, the small medical implant contains millions of lab-grown pancreatic islet cells, including beta cells, that originate from a line of pluripotent stem cells.
The devices -- approximately the size of a Band-Aid and no thicker than a credit card -- are implanted just beneath a patient's skin where it is hoped they will provide a steady, long-term regulated supply of self-sustaining insulin.
"Each device is like a miniature insulin-producing factory," said co-author Dr. Timothy Kieffer, a professor within the departments of surgery and cellular and physiological sciences at UBC, and past chief scientific officer of ViaCyte. "The pancreatic islet cells, grown from stem cells, are packaged into the device to essentially recreate the blood sugar-regulating functions of a healthy pancreas. This may have tremendous benefits over transplant of scarcely available donor-derived cells, given that we can create a virtually limitless supply."
The clinical trial was conducted at Vancouver General Hospital, with additional sites in Belgium and the U.S. Ten participants, each of whom had no detectable insulin production at the start of the study, underwent surgery to receive up to 10 device implants each.
Six months later, three participants showed significant markers of insulin production and maintained those levels throughout the remainder of the year-long study. These participants spent more time in an optimal blood glucose range and reduced their intake of externally administered insulin.
One participant, in particular, showed remarkable improvement, with time spent in the target blood glucose range increasing from 55 to 85 per cent, and a 44-per-cent reduction in their daily insulin administration.
The results are the latest in a series of clinical trials funded by Canada's Stem Cell Network and conducted by the UBC-VCH team.
"The Stem Cell Network is delighted to support this clinical trial and we're pleased to see the promising results," said Cate Murray, president and CEO of the SCN. "Moving toward a functional cure for diabetes will require a coordinated and collaborative effort. It takes excellent science by top researchers in world-leading institutions, funders, like SCN, that de-risk research, and innovative biotech companies that can manufacture and scale the technology. SCN is proud to play its part and we look forward to what's next in game-changing diabetes research."
The trials aim to accelerate the development and clinical testing of novel stem-cell based therapies for the 300,000 Canadians living with Type 1 diabetes. Diabetes is estimated to cost the Canadian health-care system $29 billion annually.
Previously, in a 2021 study in Cell Stem Cell, the researchers were the first to show that the approach could produce insulin in the human body. The latest trial sought to significantly increase the amount of insulin produced by leveraging two-to-three times more devices per participant, alongside an updated device design with small perforations to allow for blood vessel ingrowth -- a feature aimed at improving survival of the lab-grown cells.
In another ongoing trial, the UBC-VCH team is investigating whether a version of the device containing cells that have been genetically engineered to evade the immune system, using CRISPR gene-editing technology, could eliminate the need for participants to take immunosuppressant drugs alongside the treatment.
"We envision a future where people with Type 1 diabetes are able to live their lives free from daily insulin injections and free from immune-suppressing drugs," said Dr. Thompson. "That future is now within reach, and Canada is leading the way in efforts to bring these novel treatments to patients."
Stem Cells Bank Biohellenika - Web design Hexabit - W3C - Pagespeed